Are bioidentical hormones safer and more effective than traditional hormone therapy?
Since the release in 2002 of the Women’s Health Initiative report, hormone replacement therapy (HRT) used to relieve symptoms of menopause has generated worrisome, and sometimes conflicting, headlines. While linked to a reduced risk of colon cancer and fractures, the therapy has also been associated with an increased risk of breast cancer, stroke, blood clots and heart attack. And so far, there are no indications that HRT has any effect on the development of dementia.
The not-inconsiderable list of potential risks of hormone-replacement therapy has left an opening for manufacturers of “natural products” to step up with supposedly better and safer versions of hormone therapy.
There’s a lot of public interest in bioidentical (or so-called “natural”) hormone therapy for menopause symptoms. However, there’s no evidence that bioidentical hormones are safer or more effective than standard hormone replacement therapy.
Much remains unknown about these treatments for menopausal symptoms. They’re marketed as “bio-identical” hormones or “bio-identical hormone replacement therapy,” and they claim to do everything from helping menopausal women lose weight to preventing senility.
The U.S. Food and Drug Administration (FDA) warns that these claims are unproven and that the products are potentially dangerous. Bio-identical hormone replacement therapy (BHRT) is a marketing term not recognized by the FDA.
What are bioidentical hormones?
‘bio-identical’ really means that the structure of the compound is biologically identical to female hormones that are used in hormone therapy.
Some of the bio-identical hormones are “compounded,” meaning they are mixed specially to meet an individual’s needs. Bioidentical hormones are custom-mixed formulas containing various hormones that are chemically identical to those naturally made by your body. Some dyes or preservatives may be eliminated if a person is allergic to them. These prescription and over-the-counter products are marketed as being tailored to a woman’s individual hormone needs, typically determined through saliva hormone testing.
Marketers of bio-identical hormones often say the products are identical to hormones produced by the body, and these “all-natural” pills, creams, lotions, and gels don’t carry the risks of menopausal hormone therapies approved by the FDA. Agency-approved HRT drugs are typically prescribed to treat symptoms of menopause, such as hot flashes and vaginal dryness.
But be leery if a pharmacy claims that such compounded mixtures are safer or more effective than other hormone formulations. They may not be mixed according to a licensed health-care professional’s instructions.
Experts also are expressing some concerns about the products:
-
We don’t know anything about these products
-
It’s the same thing as a hormone.
-
People believe if it’s not from a drug company, it’s safe
-
Natural doesn’t always means safe
-
Over-the-counter products that are not listed as drugs (usually considered as supplements) can make some unproven claims
-
There is science behind some of what they say, but lack-of-science in many other things
The American Endocrine Society issued a position statement back in October 2006, expressing concerns about these products: “Bioidentical hormones, particularly estrogen and progesterone, have been promoted as safer and more effective alternatives to more traditional hormone therapies, often by people outside of the medical community. In fact, little or no scientific and medical evidence exists to support such claims. Additionally, many ‘bioidentical hormone’ formulations are not subject to FDA oversight and can be inconsistent in dose and purityâ€.
According to the North American Menopause Society (NAMS), custom compounds may provide certain benefits, such as individualized doses and mixtures of products and forms that aren’t available commercially. However, they may also pose risks to consumers. These compounds haven’t been approved by the FDA and as a result haven’t been tested for purity, potency, efficacy or safety. These products may even contain unknown contaminants. For this reason, NAMS does not recommend these custom-mixed products over well-tested, government-approved commercial products for the majority of women.
Also, bioidentical estrogen and progesterone are available in FDA-approved hormone therapy products, including:
Estradiol, such as Estrace, Climara patch and Vivelle-Dot patch
Natural progesterone (Prometrium)
These products come in many different doses and forms. So, you don’t need to turn to unregulated, individually compounded products as your only source of “natural” hormones.
Hormone therapy: Is it right for you?
During menopause, your ovaries decrease production of the female hormones estrogen and progesterone. This decline in hormones puts a permanent end to menstruation and fertility, but it can also cause hot flashes, mood swings, vaginal dryness and urinary problems. For decades, doctors routinely eased these symptoms with hormone replacement therapy — medications containing female hormones to replace the ones the body is no longer making. And it was widely believed that boosting estrogen levels after menopause could also ward off heart disease and osteoporosis, while improving quality of life and keeping women young.
Then, in 2002, a large clinical trial called the Women’s Health Initiative (WHI) reported that hormone therapy actually posed more health risks than benefits for women in the clinical trial. As the number of health hazards attributed to hormone therapy grew, doctors became less likely to prescribe it. And up to two-thirds of women on the therapy discontinued its use, often without talking to their doctors.
Today, there’s plenty of confusion about hormone replacement therapy, which is now commonly called hormone therapy. The truth is that hormone therapy is not the magical cure for aging that it was once believed to be, but it’s still the most effective treatment for unpleasant menopausal symptoms for most women. If you’re facing menopause, learn more about the benefits and the risks of hormone therapy.
What are the benefits of hormone therapy?
Estrogen remains the most effective treatment for relief of troublesome menopausal hot flashes and night sweats. It can also ease vaginal symptoms of menopause, such as dryness, itching, burning and discomfort with intercourse.
Long-term hormone therapy for the prevention of postmenopausal conditions is no longer routinely recommended. But women who take estrogen for short-term relief of menopausal symptoms may gain some protection against the following conditions:
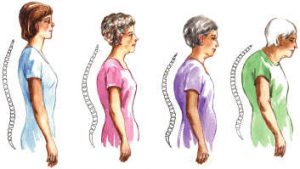 Osteoporosis. Studies show that hormone therapy can prevent the bone loss that occurs after menopause, which decreases the risk of osteoporosis-related hip fractures.
Osteoporosis. Studies show that hormone therapy can prevent the bone loss that occurs after menopause, which decreases the risk of osteoporosis-related hip fractures.
Colorectal cancer. Studies show that hormone therapy can decrease the risk of colorectal cancer.
Heart disease. Some data suggest that estrogen can decrease risk of heart disease when taken early in your postmenopausal years.
For women who undergo menopause naturally, estrogen is typically prescribed as part of a combination therapy of estrogen and progestin. This is because estrogen without progestin can increase the risk of uterine cancer. Women who undergo menopause as the result of a hysterectomy can take estrogen alone.
What are the risks of hormone therapy?
What were the results of large clinical trials on hormone therapy?
The Women’s Health Initiative found that women taking the combination estrogen-progestin (Prempro) used in the study had an increased risk of developing certain serious conditions. According to the study, over one year, 10,000 women taking estrogen plus progestin compared with a placebo might experience:
-
Seven more cases of heart disease
-
Eight more cases of breast cancer
-
Eight more cases of stroke
-
18 more cases of blood clots
Based on these numbers, the increased risk of disease to an individual woman is small. However, the overall risk to menopausal women as a group became a substantial public health concern. In addition, researchers found that women taking combination estrogen-progestin had an increase in abnormal mammograms. The higher number of false-positives (signs of possible breast cancer that ultimately prove inaccurate) was probably due to estrogen, which increases breast tissue density.
For women taking estrogen alone (Premarin), the WHI found no increased risk of breast cancer or heart disease. But researchers did find that over one year, 10,000 women taking estrogen compared with a placebo might experience 12 more cases of stroke and six more cases of blood clots in the legs, plus an increase in mammography abnormalities. This last point is important, because women who take estrogen or combination estrogen-progestin therapy may need more frequent mammograms and additional testing.
The findings of the WHI were not all bad, though. Women in the study who took combination hormone therapy experienced fewer hip and vertebral fractures than normal.
However, for most women, the exact number of blood clots and hip fractures isn’t the most important information gleaned from the WHI. The key message of this study is simply that hormone therapy shouldn’t be given to all women — like a vitamin — to make them live longer.
Who should consider hormone therapy?
Despite the inherent health risks, estrogen is still the gold standard for treating menopausal symptoms. For women who experience moderate to severe hot flashes or other menopausal symptoms, the benefits of short-term therapy outweigh the potential risks.
Data surrounding hormone replacement therapy can be scary and confusing. But the absolute risk to an individual woman taking hormone therapy is quite low — possibly low enough to be acceptable to you, depending on your symptoms. Talk with your doctor about your personal risks.
Who should avoid hormone therapy?
Women with breast cancer, heart disease or a history of blood clots should not take hormone therapy for relief of menopause symptoms. Women who don’t suffer from menopause symptoms should not take hormone therapy for preventing memory loss or strokes. Instead, talk to your doctor about other medications you can take or lifestyle changes you can make for long-term protection from these conditions.
If you take hormone replacement therapy, how can you protect yourself from the added risks?
Recent analysis of the WHI data and other trials suggests that there are several ways to reduce the inherent risks of hormone therapy. Talk to your doctor about these strategies:
Time it right. The risk of hormone therapy causing heart disease is not significantly raised in women under age 60. In fact, some studies suggest that estrogen may protect the heart when taken early in your menopausal years.
Minimize the amount of medication you take. Use the lowest effective dose for the shortest amount of time needed to treat symptoms. On the other hand, don’t be scared to continue treatment as long as you have debilitating menopausal symptoms.
If you haven’t had a hysterectomy and are using oral or skin patch hormone therapy, you will also need progestin, which is available in a pill, combination pill, vaginal gel, intrauterine device or combination skin patch. Your doctor can help you find the delivery method that offers the most benefits and convenience with the least risks and cost.
Try a form of hormone therapy with limited systemic effects. Estrogen and progestin are available in many forms, including pills, skin patches, gels, vaginal creams and slow-releasing suppositories or rings that you place in your vagina.
o   If you experience only isolated vaginal symptoms, estrogen in a vaginal cream, tablet or ring is usually a better choice than a pill or a skin patch. That’s because estrogen applied directly to your vagina is more effective at a lower dose than is estrogen given in pill or skin patch form.
o   Some studies show that the route of medication administration may affect the risk of heart disease. There is some evidence that skin patches pose less risk of heart disease than do pills.
Make healthy lifestyle changes. Counter the risks of hormone therapy by making heart-healthy lifestyle changes. Don’t smoke or use tobacco products. Get regular physical activity. Eat a healthy diet focusing on fruits, vegetables, whole grains and low-fat protein. Maintain a healthy weight. And get regular health screenings to check your blood pressure and cholesterol levels to detect early signs of heart disease.
What can you do if you can’t take hormone therapy?
Women shouldn’t have to suffer through menopause. You may be able to manage your menopausal symptoms by making healthy lifestyle choices. In fact, your doctor may recommend that you change your exercise or eating habits before you try medication. If lifestyle changes aren’t providing enough relief from bothersome symptoms, there are many medications besides hormone therapy to relieve discomfort.
The bottom line: Hormone therapy isn’t all good or all bad
Clearly, hormone replacement therapy hasn’t lived up to its billing as a panacea for age-related disease. But the news isn’t all doom and gloom either.
The only way to determine if hormone replacement therapy is the best treatment for you is to talk to your doctor about your individual symptoms and health risks. Be sure to keep the conversation going throughout your menopausal years. As researchers learn more about hormone therapy and other menopausal treatments, recommendations may change. Review your current treatments with your doctor on a regular basis to make sure they’re still your best option.
Hormone replacement therapy and heart disease: What’s the connection?
Around the world, women have a lower risk of heart disease than men. Doctors and researchers have long attributed this difference to the female hormone estrogen. And they’ve blamed the declining levels of estrogen after menopause for the increase in heart disease as women age.
For decades, observational studies seemed to demonstrate the protective power of estrogen — not just before menopause, when your ovaries produce estrogen naturally, but also after menopause, when supplied by pills, skin patches and other preparations.
In the 1980s and 1990s, doctors in the United States routinely recommended long-term hormone replacement therapy to postmenopausal women to treat menopausal symptoms and to prevent heart disease.
Then in 2002 came the Women’s Health Initiative (WHI), a large clinical trial expected to confirm the benefits of hormone therapy. Its surprise finding: Not only did postmenopausal hormones fail to protect women from heart disease — hormone therapy actually made older women more likely to have heart attacks, blood clots and strokes.
Current recommendations
Doctors no longer prescribe hormone therapy to prevent heart disease and other chronic conditions affecting postmenopausal women. Today, however, the fear of using any postmenopausal hormone therapy at all has subsided. That’s partly because continuing analysis of WHI data points to a middle ground rather than an all-or-nothing approach to hormone therapy.
It’s also still possible that hormone therapy confers some protection from heart disease when taken early in your postmenopausal years. A randomized, controlled clinical trial — the Kronos Early Estrogen Prevention Study (KEEPS) — exploring estrogen use and heart disease in younger postmenopausal women is under way, but it won’t be completed for several years.
What should you do?
To an average woman, the added heart risk from hormone therapy is no cause for alarm. Your individual risk of developing heart disease depends on many factors, including family medical history, personal medical history and lifestyle choices. Talk to your doctor about your personal risks, may be they aren’t significant enough to preclude hormone therapy for menopause symptoms.
But if you already have heart disease or you have a history of blood clots, proceed with caution. Work with your doctor to find the safest, most effective treatment for your menopause symptoms.
Women of all ages should take heart disease seriously. It’s the leading cause of death for women 65 and older, the third-leading cause of death for women 25 to 44 and the second-leading cause of death for women 45 to 64.
At the same time, most women can safely take short-term hormone therapy for menopausal symptoms without significantly increasing the risk of heart disease. If you experience severe vaginal symptoms or wake up at night with hot flashes, don’t avoid hormone therapy for fear of its risks. Instead, talk to your doctor about how you can relieve troublesome symptoms while protecting your heart.
About Dr. Suzan Gharaibeh
 Dr. Suzan Gharaibeh has recently joined Abu Hammour Medical Center in Dubai Healthcare City from the faculty at Southern Illinois University School of Medicine, where she was engaged as an assistant professor of endocrinology, diabetes and metabolism.
Dr. Suzan Gharaibeh has recently joined Abu Hammour Medical Center in Dubai Healthcare City from the faculty at Southern Illinois University School of Medicine, where she was engaged as an assistant professor of endocrinology, diabetes and metabolism.
Dr. Gharaibeh completed a two-year endocrinology fellowship at SIU School of Medicine (2007). She completed her internal medicine residency at the Hospital of Saint Raphael/ Yale University School of Medicine in New Haven, Conn. (2005). She earned her medical degree from Jordan University of Science and Technology in Irbid, Jordan (2000).
Gharaibeh is American Board certified in Internal Medicine and American Board Certified in Endocrinology, Diabetes, and Metabolism. Her memberships include the Endocrine Society and the American Association of Clinical Endocrinologists. She is certified by both to perform thyroid ultrasounds and fine needle aspiration biopsies. Gharaibeh’s research interests include diabetes, thyroid disorders and parathyroid dysfunction/osteoporosis.
For further information, please contact Dr. Suzan Gharaibeh
Email:drgharaibeh@yahoo.com.
Abu Hammour Medical Center
Dubai Healthcare City
Office Phone: +97143635353
Office Fax: +97143635354































